This prevalent issue is frequently overlooked or misinterpreted. Pelvic organ prolapse, a disease in which the uterus, bladder, small intestine, or rectum bulges into the vaginal wall or drops down through the vagina, affects around half of the women over 50. However, unlike other prevalent health issues, many women are reluctant to discuss it, even with their doctors. Some people do it out of embarrassment, while others do it because they believe it's simply something they'll have to cope with as they get older.
Pelvic organ prolapse conditions
Normal positions of pelvic organs

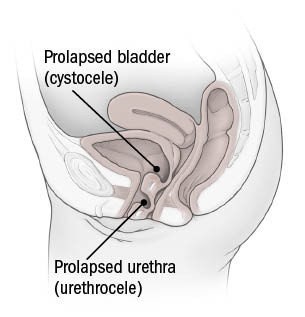
Cystocele and urethrocele
Rectocele

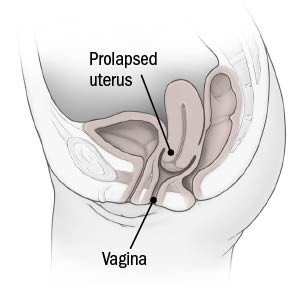
Uterine prolapse
Prolapse symptoms
The bowl-shaped structure of muscles and ligaments inside the pelvis weakens, allowing one or more organs to move lower and protrude into the vagina. Often, there are no signs, and the lady is unaware that it has happened. However, in certain cases, this movement compresses pelvic tissues, causing urinary issues or constipation. Women may have pelvic pain or a protrusion in the vaginal area. Sex may be excruciatingly painful.
The stress of pregnancy or delivery might cause these issues. Pelvic organ prolapse is more common after a vaginal delivery, although it may also happen after a cesarean. Older age, being overweight, and having a disease that causes frequent coughing, which exerts downward pressure on the pelvis, are all risk factors for pelvic organ prolapse. If your mother or another close family has experienced pelvic organ prolapse, you may be more susceptible to it.
Types of Organ Prolapse
The location of the issue, whether at the front (anterior) or rear (posterior) of the pelvis, determines the specific symptoms of prolapse.
The most frequent kind of pelvic organ prolapse is anterior vaginal wall prolapse. The bladder can slip down (cystocele) due to loose tissues in the front of the pelvis, squeezing the urethra, the tube that transports urine from the bladder out of the body (urethrocele).
The small intestine (enterocele) or the rectum may be involved in posterior vaginal wall prolapse (rectocele). Rectocele is not the same as rectal prolapse, which occurs when the rectum protrudes through the anus.
Another prevalent disease is uterine prolapse, which occurs when the uterus and cervix separate.
Apical prolapse, also known as vaginal vault prolapse, occurs when the top section of the vaginal wall sags after a hysterectomy.
Not everyone who has a prolapsed pelvic organ is disturbed by it. During a pelvic exam, your gynaecologist may notice prolapse. There's no need to be alarmed or address the disease if you don't notice it. Prolapse is nearly never a life-threatening condition. One uncommon exception is if a woman suffers full uterine prolapse, in which the organ protrudes beyond the vaginal entrance and extends a few inches beyond it. It can squeeze the urethra in this position, preventing urination and causing kidney issues. According to Dr Von Bargen, medical therapy is required.
Important health read: 10 TIPS TO ENSURE YOU AGE GRACEFULLY.
Treatment of prolapsed pelvic organs
Women who are experiencing symptoms of pelvic organ prolapse should seek medical help. Choosing amongst the different treatment choices is frequently a personal choice.
Each choice has advantages and disadvantages, and choosing between them is a highly personal decision. Some women want to get rid of the problem as soon as possible and choose surgery, while others wish to avoid surgery's hazards and opt for other options.
The following are some of the treatment possibilities for pelvic organ prolapse:
Physical treatment for the pelvic floor. This method improves the pelvic muscles, allowing them to better support the organs and, ideally, reversing or reducing prolapse. You will work with a physical therapist who specializes in helping women strengthen their pelvic floor if you choose this option.
Pessary. A pessary is a support device that looks like a diaphragm for birth control (although a pessary is not designed to prevent pregnancy). It is placed into the vaginal canal and supports the pelvic tissues that are drooping. However, it is not a cure. The prolapse will return if the device is removed. A pessary can be utilized in a variety of ways. Older women who aren't comfortable putting the device in or out can have it placed by a doctor and remained in for three to six months at a time.
A pessary is a detachable device that supports the pelvic organs temporarily.
For sexual intercourse, several forms of pessaries must be removed. Some women prefer a self-managed device, which they can put in and out themselves, for these and other reasons. This allows a woman to utilize it whenever she wants, such as during exercise. Others may wear it during the day and take it off at night. If prolapse bothers you all of the time, you can leave it and simply take it out once a week. Because vaginal discharge can build up around the device, removing the pessary on a regular basis helps it to cleanse. A pessary will not induce a vaginal infection like bacterial vaginosis or yeast infection, but the discharge might be bothersome.
Surgery. Physical therapy or a pessary may not be effective for some women, so they choose to have the issue surgically corrected instead.
Prolapse surgery aims to tighten the ligaments and muscles that cause the pelvic organs to fall out of place. Your surgeon will use a specific mesh or your own tissues to strengthen the weaker areas.
This can be done using a variety of surgical procedures, and the operation may be performed differently depending on the type of prolapse you have.
Pelvic organ prolapse surgery may or may not include a hysterectomy. A hysterectomy, on the other hand, is insufficient to correct prolapse. The actual issue is laxity in the ligaments that hold the vaginal walls in place. When logistically possible, keeping the uterus in situ has benefits such as less blood loss, a quicker operation, and a speedier recovery. However, the surgeon may need to remove the uterus in order to reach the tissues that need to be tightened, or a woman may need a hysterectomy for other reasons.
If a woman is no longer sexually active and has no desire to be, she may choose an obliterative surgical surgery, in which the vagina is permanently narrowed or closed to preserve the organs in place.
Related topics: VAGINAL ATROPHY (ATROPHIC VAGINITIS).

