We are led to assume by advertisements that vaginal probiotics, like douches, will somehow improve our health or make us feel "cleaner." Some ads say that these products help prevent or treat things like yeast infections, bacterial vaginosis, and urinary tract infections.
Women screened early are less likely to develop colorectal cancer.
A new study shows that women who start testing for colorectal cancer at 45 are much less likely to get the disease than those who don't test or who start testing at 50. The study's results, which were published online by JAMA Oncology on May 5, 2022, back up new national guidelines that say colorectal screening should start at age 45 instead of 50. This is because the number of young adults with colorectal cancer has gone up by 50% over the past 50 years.
The study, directed by Harvard researchers, analyzed 111,801 women (average age: 36) from the Nurses' Health Study II who were followed from 1991 to 2017. Every two years, participants reported whether or not they had undergone a colonoscopy or sigmoidoscopy, examinations that use a flexible tube and a camera to examine the colon and rectum. The tests allow doctors to find cancers early on and remove polyps that could turn into cancer.
Vaginal odour, itching, or burning. Irritants, such as perfumed pantyliners or new soap, can temporarily trigger these symptoms. But if they recur frequently or worsen, your doctor may want to check for a sexually transmitted or vaginal infection.
Menstrual changes. Even though irregular periods are common during perimenopause, your physician will want to know if your menstrual cycles occur more frequently than every 21 days. She will also investigate if your menstrual cycles have become noticeably heavier or longer.
Pelvic discomfort or pain. Menstrual cramps and occasional pelvic twitches are normal. However, if pain or discomfort, including bloating, worsens over time, you should speak up. Uterine fibroids, endometriosis, ovarian cysts, and (rarely) cancer are potential causes.
New bleeding. If you haven't had a period for at least a year, unexpected bleeding could indicate uterine cancer or another potentially serious condition. An ultrasound or biopsy may be necessary.
Good gynaecological care, as this type of medical care is known, is essential for a variety of reasons. Depending on your needs and insurance coverage, you may receive gynaecological care from a gynaecologist, a primary care provider (PCP), such as a doctor or nurse practitioner, or a nurse practitioner. Consider this post "Gynecare 101. In it, I will describe the fundamental reasons for a gynaecological care visit and how to choose between a gynaecologist and a primary care physician. I will also talk about what happens during a visit to a gynecologist, what will be talked about, and how to make the visit as comfortable as possible.
A Pap smear to help prevent cervical cancer (this screening test examines cells on the cervix for abnormalities or precancerous changes);
If you have symptoms of a urinary tract infection (UTI), such as burning when you urinate, cloudy or bloody urine, urinating more frequently than usual, or having an intense urge to urinate, consult your doctor.vulva (outer portion of the vagina) rashes, bumps, or irritationSymptoms of perimenopause or menopause, such as irregular periods, hot flashes, or vaginal dryness.
Should you visit a general practitioner or a gynaecologist?
Numerous primary care teams, particularly family medicine practitioners, are equipped to provide fundamental gynaecology care. They can do Pap smears and test for STIs, give you medicine or advice for UTIs, vaginal infections, and urinary tract infections, and help you choose the best way to prevent pregnancy.
Nevertheless, a gynaecologist is the best person to address certain issues. For instance, you should consult a gynaecologist if you have a vaginal discharge.
Periods that are painful or irregular
Severe pelvic pain or pain during sexual activity.
Consult a gynaecologist about birth control if you want to use long-acting methods, such as an intrauterine device (IUD) or a birth control implant, or if you have certain health conditions, such as high blood pressure or lupus, that make certain birth control methods unsafe for you.
What occurs during a visit for gynaecological care?
As with any physician, a gynaecologist will inquire about your medical history. They will also inquire about your sexual history, including when you first had sex and whether you are sexually active, as well as your desire to have children.
When I see a new patient for a gynaecological exam, I perform a comprehensive examination that includes a breast exam, an abdominal exam, and a pelvic exam. The vulva and labia (lips) that form the outer genitalia, inner thigh, and buttocks are examined during a pelvic exam. I then use a speculum to examine the vaginal tissues. This examination may be slightly uncomfortable due to a feeling of pressure, but it should not be painful. Always inform your provider if you are experiencing pain during the examination.
If you have symptoms, you may be tested for vaginal infections, sexually transmitted infections, or urinary tract infections. Any vulvar skin issues may necessitate a small skin biopsy or lesion sample.
What Are Postnatal Vitamins?
Principal Ingredients in Postnatal Vitamins
Getting the right nutrients is crucial for mothers both during and after pregnancy. While postnatal vitamins give you the micronutrients you need after giving birth, prenatal vitamins are taken during pregnancy. The major nutrients in postnatal vitamins are shown below.Omega-3 Fatty Acids
For a healthy brain, eye, and nerve cell development in developing infants, omega-3 fatty acids are essential, particularly the longer chain DHA (docosahexaenoic acid) found in fish or algal oils. There is some evidence that taking fish oil supplements can also help with mood and stress management after giving birth.Choline
An essential vitamin for a healthy infant's brain and memory development is choline. Choline requirements rise during pregnancy and are greatest for breastfeeding mothers. Additionally, choline helps maintain digestive and immunological health in pregnant women.Eggs, organ meat, caviar, salmon, shitake mushrooms, and soybeans are among the foods high in choline. A postnatal vitamin containing choline is a good substitute if some of these items are a little too exotic for you to regularly eat.
For the first year after giving birth, lactating moms are advised to take 550 mg of choline daily.
Due to blood loss after childbirth, iron levels can drop. Iron is a crucial mineral for breastfeeding mothers to restore for both themselves and their children.
Iron helps your baby's thyroid function develop properly. To generate haemoglobin, a protein that delivers oxygen to your red blood cells, your body needs iron. You can get iron deficiency anaemia if your haemoglobin is low due to low iron levels. You experience fatigue and poor energy when you have anaemia, which can influence your mood and make it more difficult to form a bond with your child. Additionally, you can become more agitated and more prone to postpartum depression.
Cereal with iron added, lentils, lima beans, oysters, and chicken liver are a few examples of foods high in iron. A good source of iron is a postnatal vitamin.
It goes without saying that you are not the only person who has an autoimmune condition. There are more than 80 autoimmune diseases. Lupus, rheumatoid arthritis, and multiple sclerosis affect about 7% of Americans.
Fortunately, there are a variety of secure and reliable birth control methods available for those who want to avoid getting pregnant. Each has significant benefits and drawbacks to consider (see the Harvard Health Birth Control Center for details). But if you have lupus, there are other things you should talk about with your health care team, such as:
How active or aggressive is your disease? Deep vein thrombosis and pulmonary embolism are two types of potentially harmful blood clots that can develop when lupus is active. You may become more prone to developing blood clots if you use birth control that contains oestrogen, such as many birth control pills, the ring, and the patch. So, a birth control pill without oestrogen or an intrauterine device (IUD) might be safer.
Are there any antiphospholipid antibodies in your blood? These antibodies may also make you more likely to develop a risky blood clot. People with these antibodies should not take estrogen-containing birth control, even if their lupus is dormant.
What birth control methods do you favour and have you used them before? Some people favour the most sensible course of action (such as an IUD or birth control implant). Others might prefer a condom or a diaphragm because they want to avoid surgery or medications. If a particular method of birth control, like condoms, didn't work to prevent conception in the past, you might prefer a different one moving forward. Talking with your medical team about your preferences and past experiences could help you make a choice you feel good about.
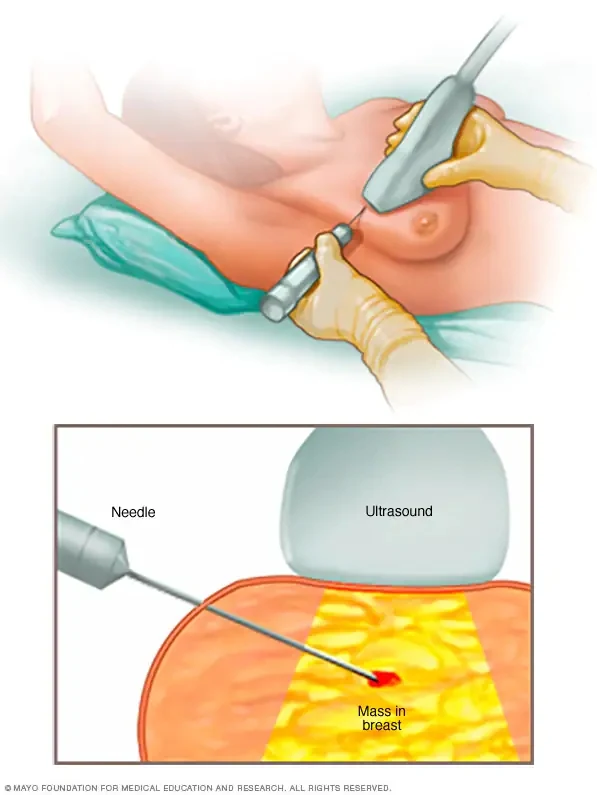
A biopsy is a sample of tissue taken from the body and inspected under a microscope. A doctor performs a breast biopsy to remove tissue from a problematic location so that a pathologist may assess whether the sample contains malignant cells.
What Is It Used For?
Why is it considered a luxury to use period products?
Protect yourself from chronic inflammation's harmful effects.
Why is it vital to talk about period stigma?
While you normally love having sex with your partner, lately you haven't been able to get off. They know your vagina like the back of their hand but nothing seems to work. What is going on here? There could be many different problems. Thankfully, a great vibrator could help you out here.
Is Your Partner Letting You Down?
You love your partner and your intimate times together. However, you haven't been able to get off lately and you aren't sure what is going on. They do everything that you like and you find them incredibly attractive. But there's just something that's holding you back from this emotional connection.
What is happening here? There are many different things that may affect your sexual drive and cause you to lose all pleasure. Not all of them are your partner's fault, either. Some may be tied more to your overall emotional and physical health. For example, you may be experiencing problems like:
- Anxiety: High anxiety, especially related to sex, may make it hard to get off. This ironic cycle is a hard one to beat. You may struggle to get off one time, feel nervous about it the next time, and find yourself continually unable to orgasm. It isn't your fault: that's just how the mind works sometimes.
- Depression: Have you felt depression about anything lately? If so, you might have a lower sex drive than anticipated and could struggle to get off. This depression is often quite hard to combat and may affect other aspects of your physical health, including your appetite and energy levels.
- Health Concerns: Some health problems may make it hard for women to orgasm, such as high blood pressure and much more. If you feel you're experiencing any of these problems, it is important to learn more about how they may affect your overall state of mind.
- Emotional Conflicts: Did you and your partner have a fight recently? Are you feeling upset at them about anything, and you aren't sure why? This situation can be very troubling and hard to predict and may also cause sexual dysfunction that can be hard to combat.